this time last year, i was 20 years old. i was suicidal, manic / depressive and self medicating, hard. on several very bad days, paralysed. genuinely in so much pain that i couldn’t turn my head, just lying still in bed, crying (gently).
i’m not here to sell you a miracle recovery story. i am now 21, and i still struggle with chronic pain. i’m still depressed. the drugs i’m on are prescription, but they are still drugs. they get me out of bed (which i can do now, woo!!!). but i am so much better; i am healing, not just coping.
healing is different for everyone, but I don’t think anyone would tell you that it’s easy. as a circus performer, my body is my art. i can tell my brain, everyone else, that i am ok (when i’m not) but my body won’t buy that shite. for me, healing is a very slow and frustrating journey of acceptance, that things beyond my control have hurt me, and that i have to recover before i can be the artist i want to.
the impact of traumatic events are complex, affecting our brains, bodies and emotions. however, the link between our emotional health and chronic pain often isn’t explored with survivors navigating the health system. unfortunately, it was only when i experienced debilitating pain that i began to ask questions and understand my own body, and ultimately how emotional safety was the missing ingredient for curing my pain.
according to gomes (2014), ‘trauma is an experience of extreme stress or shock that is/or was, at some point, part of life’. it is well understood that traumatic events have long term impacts on mental health, but what does it do to our bodies? opening the dialogue about the physiological experience of trauma is necessary to understand and facilitate meaningful healing for many people.
somatization is the term used to describe bodily symptoms or dysfunction after emotional distress. pain, muscle tension, nausea, sleep disturbances and immune suppression are very common presentations. simply, deep emotional hurt can be trapped in the body, well after the adverse event passes.
somatization
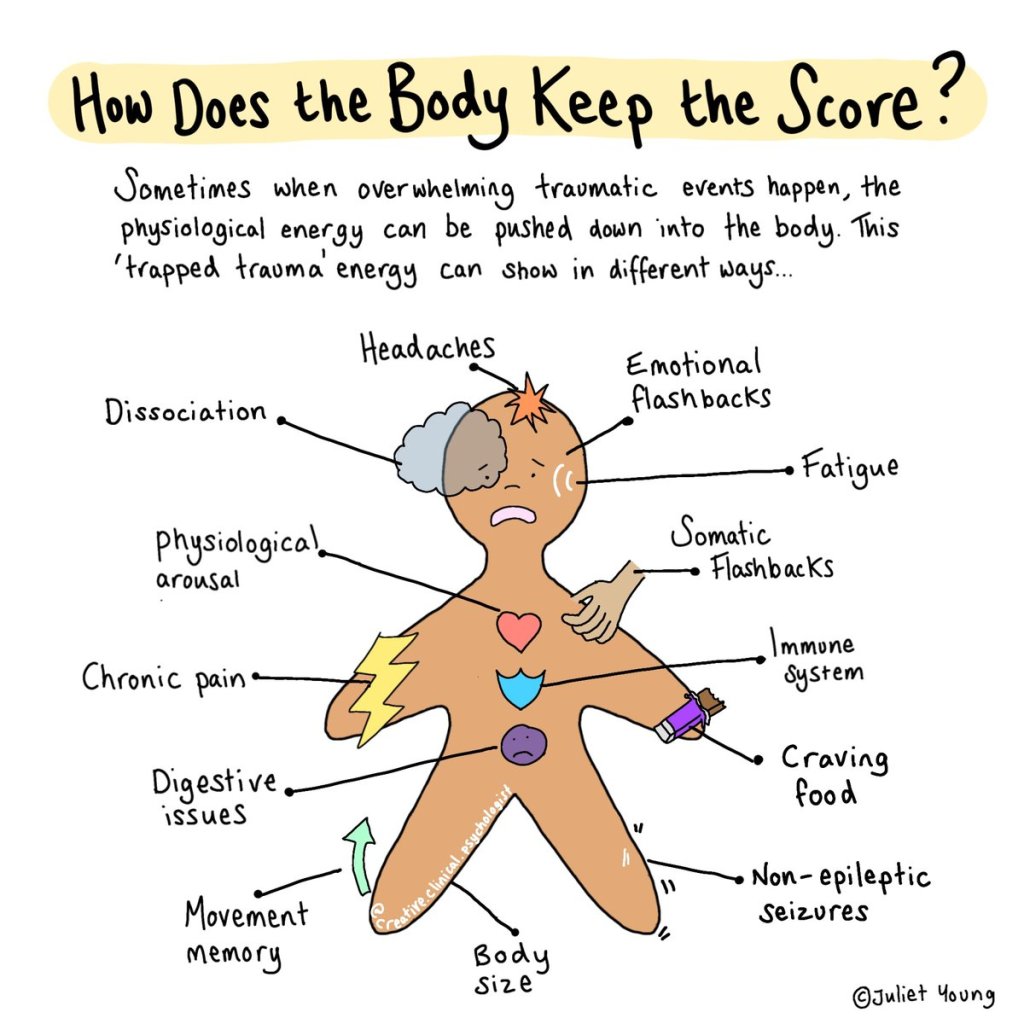
illustration by psychologist juliet young
https://twitter.com/Juliet_Young1/status/1495402247185911817
for me, understanding this finally made my experience make sense. my pain, anxiety, insomnia, low immunity did not exist in isolation from each other. i had been frustrated, on paper i was young and fit and healthy. why did I have all of these health issues? i was going to the physio every week, but my injuries were not responding. in fact, i was getting more sore and more injured.
by observing my mental states when i was in pain, it was immediately obvious… i feel pain when I am anxious or feeling out of control, when i have trauma triggers. i am very thankful to a trauma counsellor who prompted me to explore where I physically felt emotions, and walked with me as I acknowledged these sensations fully for the first time. because when you are coping, surviving, the very last thing you want to do is give in to this.
living after trauma is like driving a car while every dashboard light is on, theres a new rattle and smoke coming up from under the bonnet. you’re also on the motorway and already late… so you turn the music up keep going.
these sensations i’m talking about, stomach clenching, heart crushing fear and discomfort would be with me everywhere, everyday. of course, my body and brain had good reason to warn me that things might not be safe, but I had to get on with my life. that’s why I say when you are coping, you can’t acknowledge these sensations, you cant stop when you feel overwhelmed. you’d never do anything again.
so for me, healing began by finally listening to what my body was screaming at me. i was a mess, emotional, exhausted. and also, so much lighter. it felt so, so good to drop the mask. it was a big physical release of all that energy i had been holding.
so what is actually going on… how can we ‘hold’ emotions in our body?
traumatic events are a threat to our safety, and our brains and bodies react to keep us safe. the activation of the sympathetic nervous system (the “fight or flight” response) primes our bodies to escape dangerous situations, a complex and powerful change in our physiology. a hormonal cascade increases heart rate and shunts blood to the muscles, away from our brain and organs. we breathe faster and our blood pressure and muscle tension increases, primed to react. a sympathetic response is a short term body state, and in ideal circumstances we can remove ourselves from the situation quickly with our energised bodies. when we are removed from danger, the complementary parasympathetic nervous system will activate, returning our bodies to a calm, restful state.
but what happens when there is not a simple return to safety? traumatic events occur in the broad context of our lives; most trauma victims do not have the luxury of removing themselves from all danger or threats, so how does the body cope with that?
essentially, it doesn’t. a sympathetic nervous system that stays activated leads to hypertension, sleep disturbances, digestive dysfunction and tense, painful muscles. over time the hormonal changes responsible for the sympathetic response lead to constricted blood vessels which reduces blood flow to muscles, tendons and nerves. this leads to a decrease in oxygen in the cells, releasing pain producing chemicals (like cytokines and prostaglandins) causing further muscle tension, tissue damage and subsequent pain. stress hormones (like cortisol) involved in the sympathetic response suppress our immune systems, increase inflammation and change our metabolism. this state of hyperarousal is not sustainable, it costs a lot of energy, and if we don’t return to a safe and calm state, the body gets exhausted and enters hypoarousal.
the window of tolerance
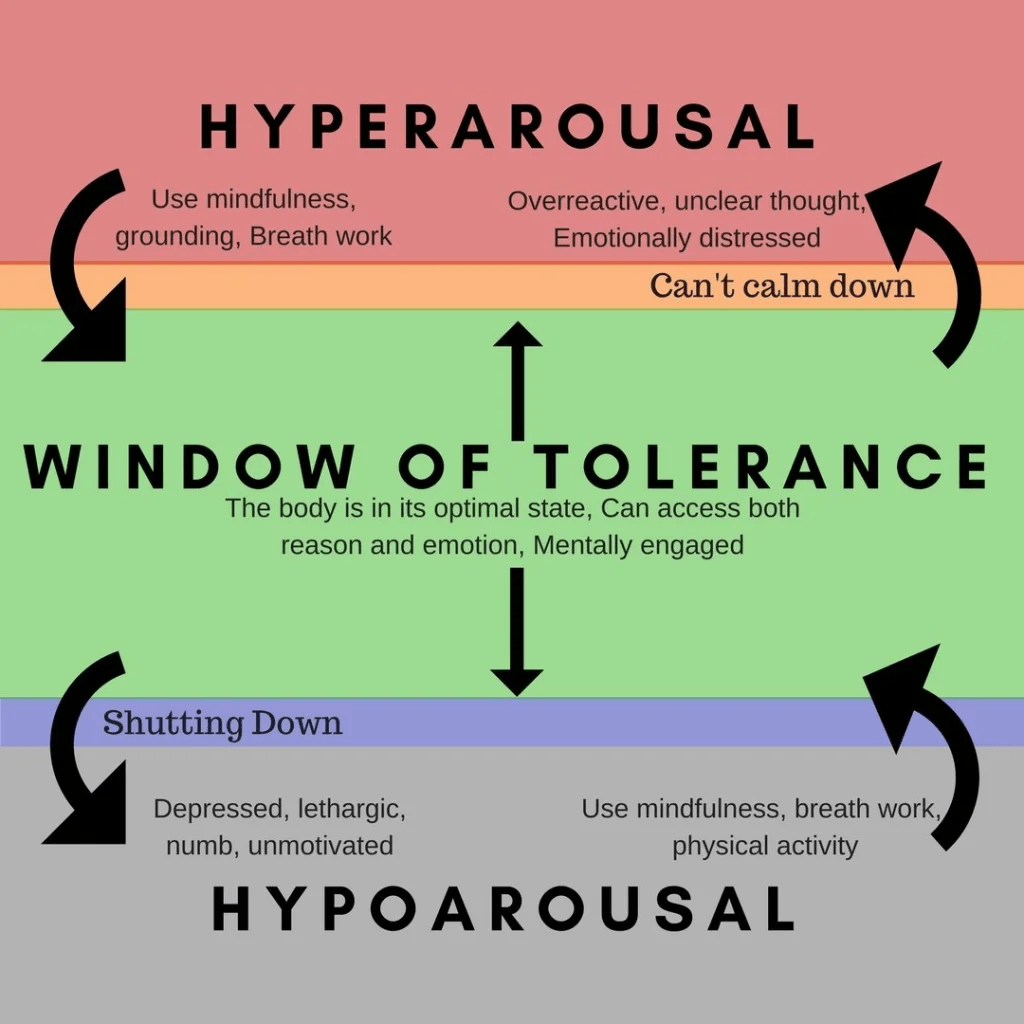
the window of tolerance is the state of optimum function, where our body is neither hyper or hypo aroused https://www.richardbamfordtherapy.co.uk/blog/window-of-tolerance/
so… this all sounds quite dire. what do we do? how do we heal our bodies? the tools are pretty simple… mindfulness, breathwork, physical activity. if we think of trauma as a situation where we have extreme lack of control, we can heal through the opposite… situations of safety, comfort, where we are in complete control and can allow our bodies to relax.
veena o’sullivan is a physiotherapist who helps trauma survivors release pain and heal from trauma. she writes about her approach as a therapist, using movement and touch, to integrate patients mind, body and emotions.
the pain and breath connection
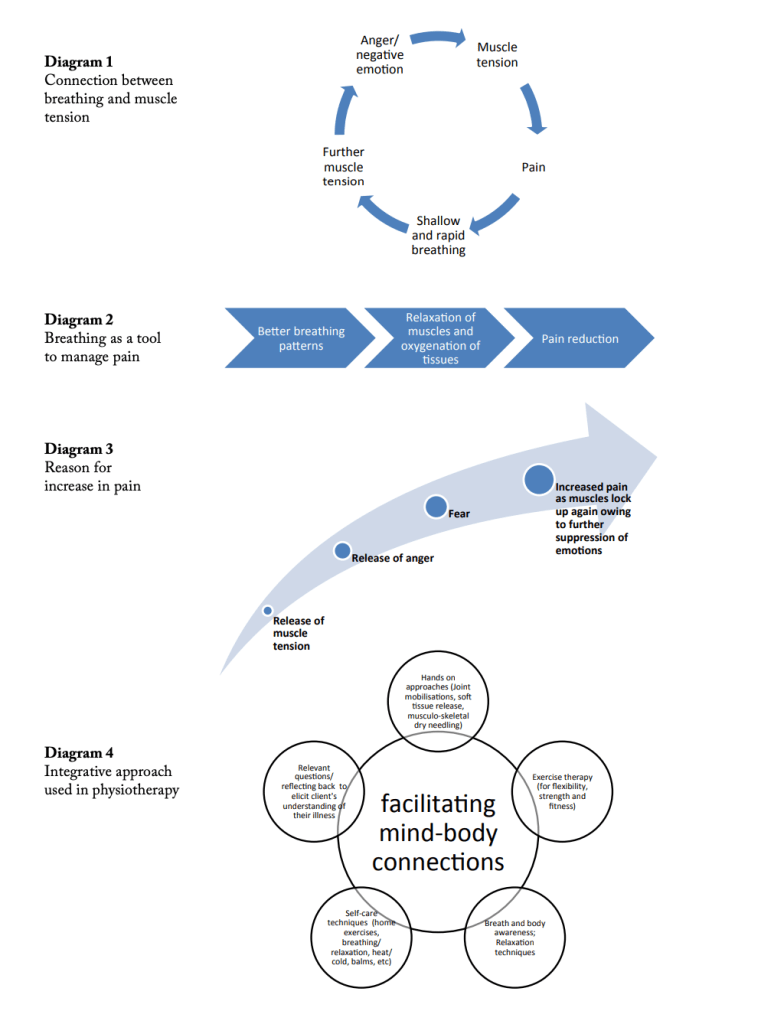
from the work of physiotherapist veena o’sullivan
https://www.startts.org.au/media/Releasing-the-Pain_Physiotherapy_Veena-Osullivan.pdf
we can use these techniques as our own healers through meditation and yoga. i am not someone who had an existing practice in either of these areas, and i absolutely benefitted just from following youtube yoga practices and guided meditations. take this advice with a grain of salt, the internet is big and not everything there is high quality… you are the best informed person to decide what is right for your body.
in my experience, this kind of work takes a lot of energy. it takes time to process and recover. i had to adjust my expectations for myself, i wasn’t able to do as much. i wasn’t as productive. i needed time off work.
this was actually the hardest part. after years of ignoring warning lights, it was pretty hard to pull over. i am very lucky to have had access to the support i needed to do this.
if you are someone living with trauma, i invite you to check in with your body. acknowledge how very resilient it is, thank it for keeping you safe. is there any way you can show it some gentleness today, a safe moment where you can hold yourself?